Carbon Dioxide (CO2)
Monitoring for Indoor Air Quality
Last review/revised: November 15, 2023
On this page…
CO2 Monitors:
- How Much Indoor CO2 is Acceptable?
- How to Place/Install a CO2 Sensor
- Increasing Ventilation and Decreasing CO2 Concentration
- Hosting or attending a social gathering? WATCH the air you breathe.
- Clean air @ Work. WATCH the air you breathe
Other Resources:
- Wildfire smoke, air quality and your health
- Where Does Indoor CO2 Come From and Why Is It Important?
- What’s the difference between Carbon Monoxide (CO) and Carbon Dioxide CO2?
- Why Ventilation and Filtration is Important
- What Do High Levels of Carbon Dioxide (CO2) Mean?
- Multiple Public Health Measures Needed
- Plexiglass barriers and indoor air quality. What do we know?
- Resources and Further Reading
Where Does Indoor CO2 Come from and Why Is It Important?
When we exhale, we add CO2 to the air. In fact, each breath from an average adult contains 35,000 parts per million (ppm) of CO2. As more people remain in a room, CO2 levels increase quickly if there is not enough fresh air coming into the space. High indoor CO2 levels can cause tiredness, headaches and other symptoms. Increasing CO2 levels show you that the space is not well ventilated. Other indoor pollutants can also increase within a poorly ventilated space. This includes respiratory particles and the viruses they carry. For example, COVID-19 spreads from person to person through droplets and airborne transmission. Due to gravity, larger and heavier droplets fall quickly. Respiratory particles spread in the air are called aerosols. Smaller and lighter aerosols remain suspended in the air longer than droplets. Viruses and pollutants can live on aerosols depending on factors such as temperature, pH, humidity, and airflow. Aerosols come from when we:
Poorly ventilated indoor spaces increase your risk of COVID-19. To be clear, the reading on a CO2 monitor is not a direct indicator of risk for COVID-19. CO2 readings will help you determine if you should take simple steps to lower the risk of transmission. This includes things like opening a window or reducing the number of people in a room.
Poorly ventilated indoor spaces increase your risk of COVID-19. The reading on a CO2 monitor is not a direct indicator of risk for COVID-19. Instead, CO2 readings can determine if changes should be made to ventilation or capacity limits. Improving ventilation and reducing the number of people inside, can decrease the risk of transmission.
What’s the difference between Carbon Monoxide (CO) and Carbon Dioxide (CO2)?
CO is a gas that is often called the silent killer because it contains no smell, colour, or taste and can cause illness or death. CO is produced when things like coal, gasoline, natural gas, oil, propane, wood, or tobacco are burned. CO risks are present year-round, but can be riskier in the winter when people are heating their homes. Other sources of CO include vehicle exhaust, BBQs, and lawn equipment.
CO2 is another gas, but is mainly produced when people exhale. Reducing CO2 can be done by increasing ventilation and decreasing the number of people in one space.
How Much Indoor CO2 is Acceptable?
Health Canada has set the long-term exposure limit for CO2 in residential settings (i.e. in your home) at 1000 ppm, averaged over a 24-hour period. However, it is normal for CO2 levels to fluctuate and serious health effects are not expected below 5,000 ppm.
For example, if you are monitoring CO2 in your home, you may see higher readings if you have friends over for a social gathering. The increase in number of people, talking and laughing increases the production of CO2. If CO2 levels begin to rise, this indicates not enough fresh air is coming in for the number of people present. Generally, you should aim to keep CO2 levels below 1000 ppm, or ideally, as close to outdoor levels as possible.
Why Ventilation and Filtration is Important
Increasing air circulation, using air filtration, and removing pollutants can improve IAQ. Risk of illness (from exhaled breath that might have viruses or bacteria in it) can be reduced with good ventilation and air filtration. Reducing the number of people in the room will also decrease risk. Air filtration units (i.e. HEPA filters*) will only remove particles from the air, not CO2.
*HEPA filter = High Efficiency Particulate Air filter
How to Place/Install a CO2 Sensor
CO2 sensors should be placed on a wall at a height of 1-2 m and well away from windows or air supply vents, and at least 2 m away from people or open flames. Once installed, you should see CO2 levels change a lot as people enter and leave the space, or when windows and doors are opened.
What Do High Levels of Carbon Dioxide (CO2) Mean?
High CO2 levels can mean that ventilation is insufficient for the number of people present, which might also be causing other IAQ issues. CO2 levels can be affected by many different things, such as:
- Age of a building (not designed with current ventilation needs in mind);
- Design of a building (built for one purpose, but now used for another);
- Function of the building (may have windows that cannot open for certain reasons)
- Size of the building (may not allow for people to spread out)
- Number of people in the building;
- Other CO2 sources, such as smoking, stoves, furnaces, water heaters, and pets.
Also consider:
- CO2 sensors can tell you if the ventilation is okay, but dangerous indoor air pollutants can still be present even if CO2 levels are low.
- Remove other sources of indoor air pollutants using Health Canada’s IAQ resources
- Wildfires, extreme heat, and other sources of outdoor pollution may impact IAQ.
- If outdoor pollution is present, indoor air filtration becomes more important
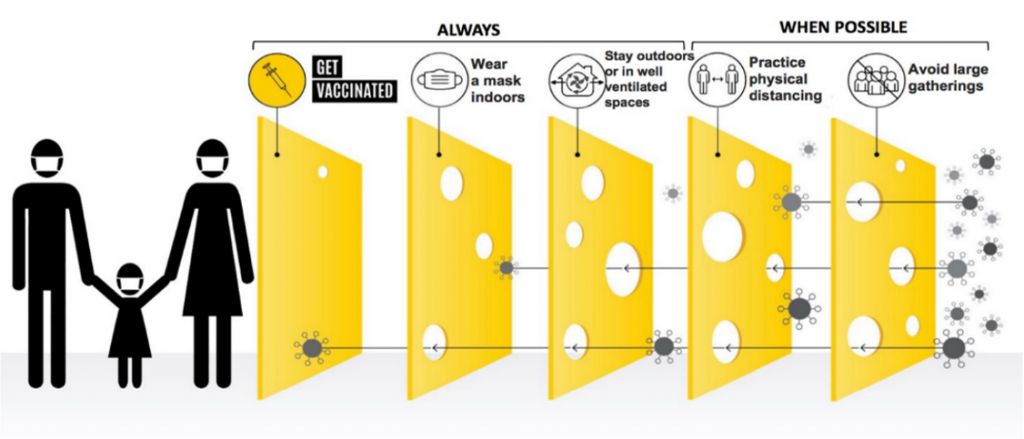
Multiple Public Health Measures Needed
It is very clear that no one prevention measure alone will reduce the spread of COVID-19. A combination of measures (or layers) are needed. Improving ventilation is just one way that may help to reduce the spread of COVID-19, indoors. This is often viewed as the “Swiss Cheese Model”, shown here.
Increasing Ventilation and Decreasing CO2 Concentration
If your CO2 monitor is showing higher levels of CO2, you may consider one or more of the following:
- Reducing the number of people in the building;
- Avoiding strenuous activities like singing, dancing, and shouting
- Servicing or upgrading your HVAC system;
- Consider using HEPA filters in your HVAC system to reduce particles in the air that may contain viruses or bacteria
- Increasing the amount of outdoor air being drawn into your HVAC system, to decrease the recirculation of ‘stale’ air;
- Placing portable air filtration systems throughout the building;
- Opening windows and doors where the safety of occupants won’t be jeopardized, and the function HVAC system won’t be affected;
- Installing screens so that windows and doors can be opened without the risk of pests (e.g. flies) coming in; and/or
- Increasing the humidity of your space.
Conclusion
Using a CO2 monitor helps to identify three kinds of risk:
- the negative effects of CO2 exposure,
- the potential for other pollutants to accumulate in a poorly ventilated space, and
- the risk of being in a poorly ventilated space during the COVID-19 pandemic.
Many factors need to be considered when a high (or low) CO2 reading is recorded. Additionally, readings need to be interpreted with caution. Simple and effective ways to improve ventilation exist, but increasing ventilation alone is not enough to stop the spread of respiratory diseases (like COVID-19) or decrease risks.
Other important strategies to reduce the spread of COVID-19 include:
- getting vaccinated,
- wearing a mask,
- maintaining physical distance from others, and
- maintaining proper hand hygiene.
We are proud to work with the Peterborough Public Library and other partners on this collaboration – a North American first, we believe – to ensure these devices are as accessible as possible to the community regardless if people could afford to access these otherwise costly devices. Special thanks to these partners that helped made this project a reality:
- Danielle J. Cane, London School of Hygiene and Tropical Medicine
- Dr. Angela Eykelbosh, Environmental Health and Knowledge Translation Scientist, National Collaborating Centre for Environmental Health
- Barry Hunt, Prescientx
- Kate Nyhan, Cushing/Whitney Medical Library, Yale University
- Dr. Comilla Sasson, Colorado School of Public Health and University of Colorado
- Cheryl White, Masks4Canada
Plexiglass barriers and indoor air quality. What do we know?
We’ve learned a great deal about COVID-19 since the pandemic began, most notably, is that COVID-19 is an airborne virus, and does not spread as easily as we once thought by touching contaminated surfaces. The Canadian Centre for Occupational Health and Safety states that “the virus that causes COVID-19 spreads from a person that is infected through the air, by respiratory droplets and aerosols.” Additionally, the Ontario Science table noted that “aerosols play a role in the transmission of SARS-CoV-2, especially in poorly ventilated indoor areas.”
Former provincial regulations, such as the Reopening Ontario (A Flexible Response to COVID-19) Act, once outlined the mandatory public health measures to prevent the spread of COVID-19. It is now understood that some measures, like environmental cleaning and installing impermeable barriers may not be as effective for containing the transmission of COVID-19 in public settings as was once thought.
The Centre for Disease Control states “When not carefully installed, barriers can sometimes hinder good ventilation.”
Public Health Ontario recently hosted a webinar and described using impermeable barriers as a ‘strategy to avoid.’
Health Canada research notes similar findings, stating “There is limited evidence related to the effectiveness of screens and barriers, which are often made of plexiglass, in reducing the risk of COVID-19 transmission.”
Additionally, impermeable barriers or screens “are more likely to be effective if individuals are face-to-face or very close together; interactions between individuals are short, so that aerosols do not accumulate; and when the barriers are appropriately sized and designed to work with the airflow of a space.”
Dr. Makoto Tsubokura of the RIKEN Center for Computational Science (R-CCS) talks about his work using the supercomputer Fugaku to simulate the spread of COVID-19 through droplets in the air in a variety of situations, such as public transportation and theaters.
Workplaces that employ regulated professions (i.e. Occupational Therapists, Physio Therapists, Registered Nurses, etc.) may wish to consult with their respective Colleges before implementing any changes.
Things to consider before adding or removing impermeable barriers or screens at your workplace:
- Do the screens or barriers impede ventilation/airflow from an open window or HVAC system?
- Is the interaction with your staff or clients short or long? (i.e. barriers may provide benefit for short term, face to face interactions)
- Is there a College or other governing body that has requirements in place for your staff or clients?
Resources and Further Reading
- Fact Sheet: CO2 Monitoring for Indoor Air Quality
- Health Canada: Carbon dioxide in your home
- Health Canada: Residential Indoor Air Quality Guideline: Carbon Monoxide
- Health Canada: COVID-19: Guidance on indoor ventilation during the pandemic
- Health Canada: Improve indoor air quality in your home
- Peterborough Fire Services: Carbon Monoxide Alarms
- National Collaborating Centre for Environmental Health: Indoor CO2 sensors for COVID-19 risk mitigation: Current guidance and limitations
- COVID-19: One Page guidance documents for Indoor Air Quality (IAQ)
- ASHRAE: Core Recommendations for Reducing Airborne Infectious Aerosol Exposure
- Public Health Ontario: Heating, Ventilation and Air Conditioning (HVAC) Systems in Buildings and COVID-19
- Use of Portable Air Cleaners and Transmission of COVID-19

